Europe should prepare for a “second wave” of coronavirus Covid-19. Deconfinement continues and experts warn that EU is not ready for second Coronavirus wave. Is Europe finally today free of corona? When and how big will be the next pandemic?
Merkel and Macron urge EU to prepare for second Corona wave!
Germany and France urged EU Chief Ursula von der Leyen to consider ways to better prepare for the next pandemic. Merkel and Macron warned Europe had fallen short against the coronavirus outbreak. Europe’s chaotic response to the coronavirus outbreak raised questions about the EU’s preparedness for pandemics. 169,207 Europeans have died and a Europe-wide approach is needed.

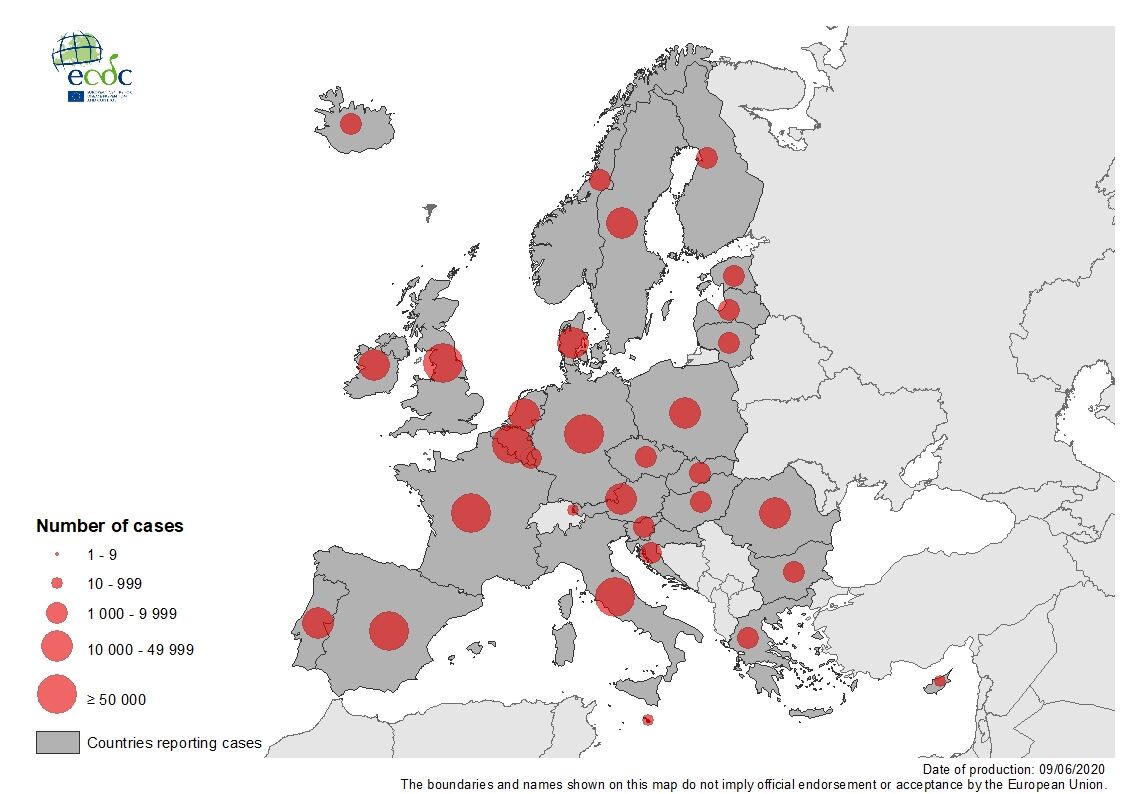
Situation update 9 June 2020, dataset collected 6:00-10:00 CET
Cases
7 069 278 Worldwide
1 444 710 in the EU/EEA and the UK
Deaths
405 587 Worldwide
169 207 in the EU/EEA and UK
EU leaders send a letter to Ursula von der Leyen in Brussels to alert EU and demand a common Coronavirus Response. The letter was signed by Emmanuel Macron – President of France, Angela Merkel – Chancellor of Germany, Mateusz Morawiecki – Prime Minister of Poland, Pedro Sanchez – Prime Minister of Spain, Sophie Wilmes – Prime Minister of Belgium and Mette Frederiksen – Prime Minister of Denmark. The 6 EU leaders, 3 men and 3 women, urge EU for a sufficient supply of personal protective equipment (PPE), medical devices, critical medicines, and vaccines. “Understanding the shortcomings is essential,” the letter adds.
We hope that the paper can serve as an inspiration for fruitful, further discussions at European level on how to ensure the EU’s preparedness for future pandemics.
COVID-19 transmission and the risk of a second Coronavirus wave
While the viruses that cause both COVID-19 and seasonal influenza are transmitted from person-to-person and may cause similar symptoms, the two viruses are very different and do not behave in the same way. Coronavirus disease (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first identified in December 2019 in Wuhan, China, and has since spread rapidly, evolving into a full-blown pandemic.
Since the beginning of the coronavirus pandemic, ECDC’s Epidemic Intelligence team has been collecting the number of COVID-19 cases and deaths, based on reports from health authorities worldwide. This comprehensive and systematic process is carried out on a daily basis. To insure the accuracy and reliability of the data, this process is being constantly refined. This helps to monitor and interpret the dynamics of the COVID-19 pandemic not only in the European Union (EU), the European Economic Area (EEA), but also worldwide.
People who are perfectly healthy are also getting severe illness and they die. Knowing what we have seen in Europe with approximately 10% of the population [infected] I think there is for me not an option to let this go. If the the other 90% would have come as well, I think we don’t want to think of this.
Dr Andrea Ammon, EU coronavirus chief
Dr Andrea Ammon is a German physician and the current director of the European Centre for Disease Prevention and Control, an European Union agency strengthening Europe’s defence against infectious disease.
COVID-19 Cases in the EU/EEA and the UK, as of 9 June 2020
Europe will see ‘second wave’. Experts warn EU is not ready for second Coronavirus wave.
There is increasing evidence that persons with mild or no symptoms contribute to the spread of COVID-19. Asymptomatic infection at time of laboratory confirmation has been reported from many settings. During a systematic screening of 143.393 residents and 139.409 healthcare workers in all Belgium long-term care facilities, 75% of 8.780 RT-PCR positives were asymptomatic at the time of nasopharyngeal sampling. Some of these cases developed some symptoms at a later stage of infection, however, the proportion of cases that will develop symptoms is not yet fully understood.
WHO: Asymptomatic transmission routes from COVID-19 patients
There are also reports of cases remaining asymptomatic but with detectable viral RNA shedding throughout the whole duration of laboratory monitoring. In a recent review, the proportion of positive cases that remained asymptomatic was estimated at 16%, with a range from 6 to 41%.
Infection prevention and control measures
People should be informed and trained on:
- hand hygiene practices;
- respiratory hygiene practices;
- use of personal protective equipment (PPE);
- physical distancing guidelines;
- cleaning and disinfection practices;
- COVID-19 symptoms (cough, fever, sore throat, myalgia and weakness, difficulty to breath, diarrhoea, nausea and vomiting, loss of taste and/or smell);
- all internal procedures in place related to COVID-19, including procedures to be followed when a possible case is identified (pathways for confirmed/possible cases to avoid contact with non-possible cases and staff); and
- guidelines for self-isolation when symptomatic.

ECDC estimates that between 15 000 and 75 000 people die prematurely due to causes associated with seasonal influenza infection each year in the EU, the UK, Norway, Iceland and Liechtenstein. This is approximately 1 in every 1 000 people who are infected. Despite the relatively low mortality rate for seasonal influenza, many people die from the disease due to the large number of people who contract it each year.
The concern about COVID-19 is that, unlike influenza, there is no vaccine and no specific treatment for the disease. It also appears to be more transmissible than seasonal influenza. As it is a new virus, nobody has prior immunity, which means that the entire human population is potentially susceptible to SARS-CoV-2 infection.
COVID-19 is a highly infectious disease caused by the most recently discovered coronavirus. Everyone is responsible for reducing the spread by taking these simple precautions. Together we can protect ourselves and all those around us of a second Corona wave.
What is the mode of transmission? How easily does it spread?
While animals are believed to be the original source, the virus spread is now from person to person (human-to-human transmission). There is not enough epidemiological information at this time to determine how easily this virus spreads between people, but it is currently estimated that, on average, one infected person will infect between two and three other people.
Respiratory Droplets
The virus seems to be transmitted mainly via small respiratory droplets through sneezing, coughing, or when people interact with each other for some time in close proximity (usually less than one metre). These droplets can then be inhaled, or they can land on surfaces that others may come into contact with, who can then get infected when they touch their nose, mouth or eyes. The virus can survive on different surfaces from several hours (copper, cardboard) up to a few days (plastic and stainless steel). However, the amount of viable virus declines over time and may not always be present in sufficient numbers to cause infection.
The incubation period for COVID-19 (i.e. the time between exposure to the virus and onset of symptoms) is currently estimated to be between one and 14 days.

We know that the virus can be transmitted when people who are infected show symptoms such as coughing. There is also some evidence suggesting that transmission can occur from a person that is infected even two days before showing symptoms; however, uncertainties remain about the effect of transmission by asymptomatic persons.
When is a person infectious?
The infectious period may begin one to two days before symptoms appear, but people are likely most infectious during the symptomatic period, even if symptoms are mild and very non-specific. The infectious period is now estimated to last for 7-12 days in moderate cases and up to two weeks on average in severe cases.
Where can I get COVID-19 tested?
If you are feeling ill with COVID-19 symptoms (such as fever, cough, difficulty breathing, muscle pain or general weakness), it is recommended that you contact your local healthcare services online or by telephone. If your healthcare provider believes there is a need for a laboratory test for the virus that causes COVID-19, he/she will inform you of the procedure to follow and advise where and how the test can be performed.
Is there a vaccine against the virus?
There are currently no vaccines against human coronaviruses, including the virus that causes COVID-19. This is why it is very important to prevent infection and to take measures to contain further spread of a second Coronavirus wave.
How long will it take to develop a vaccine?
The development of vaccines take time. Several pharmaceutical companies and research laboratories are working on vaccine candidates before the second Coronavirus wave. It will, however, take many months or even years before any vaccine can be widely used, as it needs to undergo extensive testing in clinical trials to determine its safety and efficacy. These clinical trials are an essential precursor to regulatory approval and usually take place in three phases. The first, involving a few dozen healthy volunteers, tests the vaccine for safety, monitoring for adverse effects. The second, involving several hundred people, usually in a part of the world badly affected by the disease, looks at how effective the vaccine is in the field, and the third does the same in several thousand people.

What is the situation in Europe at the moment?
The COVID-19 pandemic is posing an unprecedented threat to the EU/EEA countries and the UK, which have been experiencing widespread transmission of the virus in the community for several weeks. In addition, there has been an increasing number of reports of COVID-19 outbreaks in long-term care homes across Europe with high associated mortality, highlighting the extreme vulnerability of the elderly in this setting.
The absence of an effective treatment or a vaccine combined with an exponential growth in infections from late February led many countries to implement non-pharmaceutical interventions such as “stay-at-home” policies (recommended or enforced), jointly with other community and physical distancing measures such as the cancellation of mass gatherings, closure of educational institutions and public spaces.
What are the travel restrictions in the European Union?
Travel has been shown to facilitate the spread of COVID-19 from affected to unaffected areas. Travel and trade restrictions during a public health event of international concern (PHEIC) follow the International Health Regulations (IHR). Most EU countries have applied national borders closure and/or border checks and travel and transport restrictions or bans within their national borders and between different regions as a measure to slow the spread.
EU “blacklist” of airports to save Safe Summer holidays

See the measures implemented by EU Member States.
How prepared is Europe for COVID-19?
The outbreak of COVID-19 has evolved dramatically in the EU/EEA and the UK. The rapid escalation of cases in several countries has placed enormous pressure on healthcare systems, and presented a major challenge for local services. All countries in the EU have responded to the emerging situation. The situation continues to evolve and lessons are still being learnt and countries are working hard to adapt their response to the ever changing situation.
The European Centre for Disease Prevention and Control (ECDC) is in continuous contact with the European Commission and the World Health Organization (WHO) regarding the assessment of this outbreak.
When can we return to normal?
The stay-at-home and physical distancing measures that have been imposed throughout the EU/EEA and the UK are highly disruptive to society, both economically and socially, and there is very wide agreement that they should be lifted as soon as it is safe to do so. However, lifting the measures too early or too quickly carries the risk of a rapid return to high infection rates, and this could overwhelm the health system while causing high levels of illness and many deaths.
The Joint European Roadmap towards lifting COVID-19 containment measures addresses this issue by providing the framework for an economic and social recovery plan for the EU alongside a set of public health principles that are aimed at minimising the risk of a resurgence in the number of cases. Should a resurgence occur, the stay-at-home and physical distancing measures may need to be put in place again.
EU countries reopen Schengen Borders for Summer Travellers

Coronavirus “free” – Safe Travel Summer destinations in Europe
The virus is around us! Not if but when?
It is increasingly recognised that we will be living with COVID-19 for many months, or even years. This disease will continue to affect our lives for some time to come, and we all need to prepare mentally for that.
Second Coronavirus Wave
Europe has avoided a significant resurgence of Covid-19 cases. Most EU countries have emerged from lockdown and restarted chunks of their economies. On the other hand the prospect of a second wave of coronavirus infection across Europe is no longer a distant theory! The question is when and how big it will be! European governments have started easing their lockdown restrictions.
Are we ready to face a second Corona wave?
Which is the way to hold the pandemic in check by less stringent means?















